
Sween 24 Once a Day Cream
Sween 24 is a moisturizing cream formulated with dimethicone to soothe dry, chapped or chafed skin and lips for up to 24 hours. As both

Living with incontinence can be challenging. One of the most uncomfortable side effects is incontinence-associated dermatitis (IAD). This condition, which often includes skin irritation and inflammation, affects many individuals with bladder or bowel control issues.
In this guide, we’ll explore what IAD is along with its causes and symptoms. Most importantly, we’ll review how to treat it and some tips to prevent it from showing up in the first place.
Incontinence-associated dermatitis occurs when skin is exposed to urine or feces for prolonged periods. This exposure can lead to inflammation, redness, and discomfort in the affected areas. IAD is particularly common among older adults, individuals with limited mobility, and those in long-term care facilities.
The short answer is yes, urine can indeed cause a rash. When skin comes into prolonged contact with urine, it can lead to IAD. The symptoms of this condition include:
These symptoms typically appear in areas directly exposed to urine, such as the genital area, buttocks, and inner thighs.
Acidic urine is a significant contributor to skin irritation and itching associated with IAD. When urine is too acidic, it can break down the skin’s natural protective barrier, making it more vulnerable to irritation and increasing skin permeability. This allows irritants to penetrate the skin more easily, causing itching and discomfort.
This stresses the importance of proper skin care and treatment of IAD symptoms. With that being said, if you’re experiencing persistent itching or discomfort, it’s crucial to consult with a healthcare provider for appropriate diagnosis and treatment.
Treating urine skin irritation and IAD involves a multi-step approach aimed at protecting and healing the skin. Here’s a comprehensive guide to managing this condition:
When dealing with the burning sensation caused by acidic urine, consider these additional steps:
Treating an incontinence rash, or IAD, in adults requires patience and consistent care. In addition to the steps mentioned above, consider these tips:
Remember, while these treatments can be effective, persistent or severe cases of IAD should be evaluated by a healthcare professional. They can provide personalized treatment plans and rule out other potential skin conditions.
While treating IAD is important, prevention is even better. Here are some strategies to help prevent incontinence-associated dermatitis:
If you’re struggling with incontinence-associated dermatitis or have concerns about skin irritation related to incontinence, don’t hesitate to reach out to your healthcare provider. They can offer personalized advice and treatment options tailored to your specific needs.
Living with incontinence and managing IAD can be challenging, but with proper care and attention, it’s possible to maintain healthy skin and improve quality of life.
When it comes to IAD, many individuals face similar challenges. Remember, numerous resources and products are available to help manage these conditions effectively.
Medical Monks is here to support you on your incontinence care journey. We stock a wide range of supplies specifically designed for managing incontinence and related skin conditions, including:
Our knowledgeable professionals are always available to help you choose the right products for your needs. We understand that every individual’s situation is unique, and we’re committed to providing personalized assistance to ensure you get the most effective care possible.
Don’t hesitate to contact us if you need help selecting appropriate supplies or have questions about managing incontinence-associated dermatitis. Our team is well-versed in the latest care techniques and products, and we’re here to provide guidance and support.

Sween 24 is a moisturizing cream formulated with dimethicone to soothe dry, chapped or chafed skin and lips for up to 24 hours. As both

Hibiclens® is a 4% chlorhexidine gluconate (CHG) based solution designed to reduce infection rates in medical facilities. This antiseptic skin cleanser and soap is designed
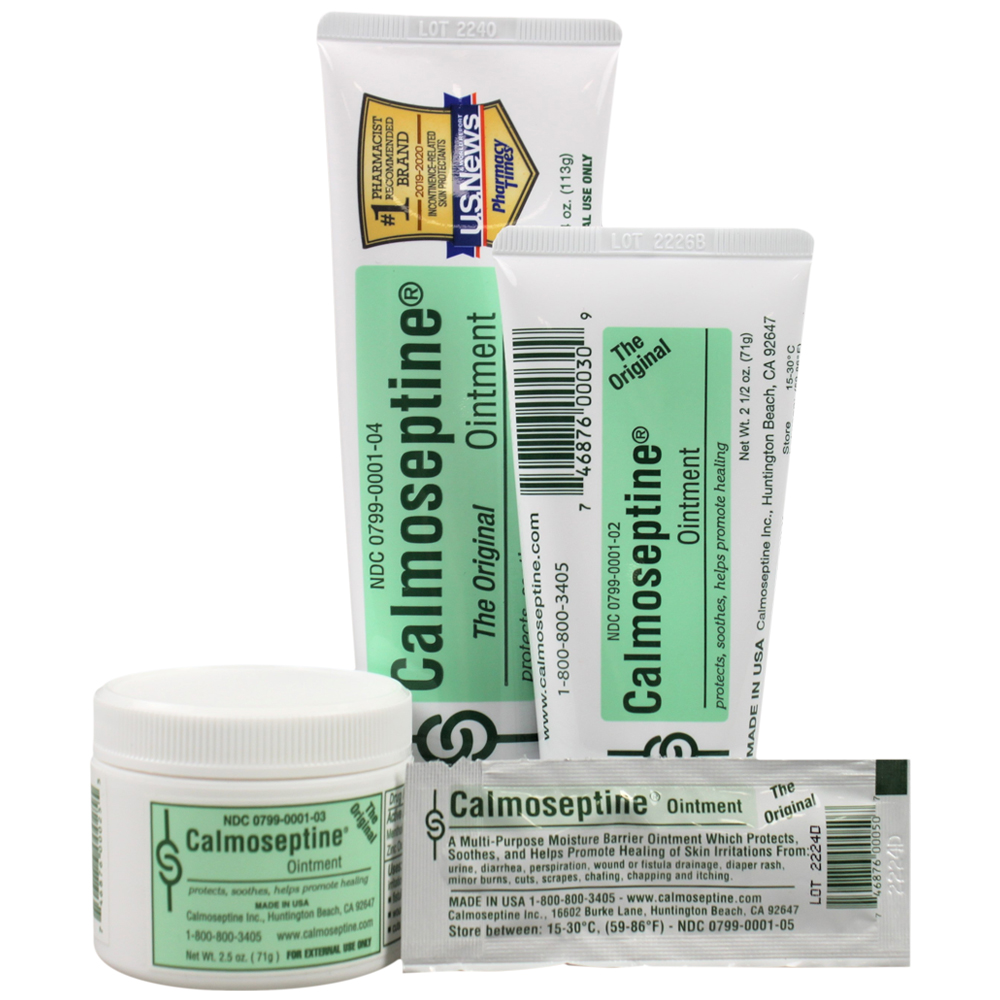
Calmoseptine® has been the topical ointment of choice for over 70 years. Whether you’re treating diaper rash, soothing an insect bite or addressing complications from

3M’s Cavilon Advanced Skin Protectant creates a waterproof, flexible barrier that helps prevent Incontinence Associated Dermatitis (IAD), reduces the need for reapplication and improves upon

Are you dealing with irritated skin? It could be sensitive, red, or dry – or

Dry skin is a common ailment that can occur due to a lack of moisture,

If you’re living with dry skin, standard moisturizers and skin care products might not be
